Companies are engineering B cells to produce gene-encoded medicines, but clinical proof of concept is needed to convince the doubters that this platform can deliver.
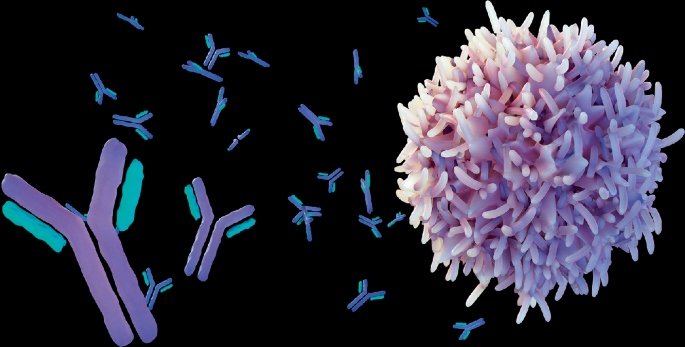
Early observations from the world’s first clinical trial of B cell ‘biofactories’, engineered to produce therapeutic proteins continuously inside a person’s body, has given the field grounds for optimism. These B cells are taken from a patient and engineered in the lab such that, once differentiated into antibody-producing plasma cells — how they would normally respond to invading pathogens — they instead make therapeutic proteins. These medicines made in situ require neither immunosuppression nor lymphodepletion and could offer developers a way to deliver genetic cargoes across a whole range of conditions that is safer and less cumbersome than current approaches.
B cells that differentiate into plasma cells secrete huge amounts of antibodies to fight infection, and could be induced to produce other therapeutic molecules.
Credit: LoveEmployee / Alamy Stock Photo
Immusoft was first into the clinic with an engineered B cell therapy (Table 1). A phase 1 trial started late last year of its lead program, iduronicrin genleukocel-T (ISP-001), in patients with mucopolysaccharidosis type I. It involves the delivery of B cells engineered ex vivo to express α-l-iduronidase, the lysosomal enzyme whose absence causes the fatal genetic condition. “We’re getting encouraging data on our first patient. We’ve seen excellent safety after reinfusing the cells, without any use of conditioning, as well as initial pharmacodynamic effects,” says Immusoft CEO Sean Ainsworth.
Table 1 Engineered B cell therapies in development
Later this year, Be Biopharma aims to become the second firm to move an engineered B cell therapy into clinical development, for treating hemophilia B. It will shortly submit to the US Food and Drug Administration an Investigational New Drug (IND) filing for testing BE-101. This treatment comprises patients’ B cells modified ex vivo using CRISPR–Cas9 to express the Padua variant of the F9 gene, which encodes a highly active form of coagulation factor IX (FIX).
These pioneering programs will provide early insights into the potential of these long-lived B cell factories to improve the delivery of therapeutic proteins. The clinical possibilities appear to be vast, given the various shortcomings of classical enzyme replacement therapy, antibody therapy, gene therapy and different forms of cell therapy. These include suboptimal pharmacokinetic profiles and dosing regimens, immunological barriers to redosing, and the need for immunosuppression (in the case of systemically administered gene therapies employing viral vectors) or harsh preconditioning regimens (required for engineered T cell, natural killer cell and hematopoietic stem cell therapies).
Developers aim to harness B cells’ intrinsic ability to produce and secrete large quantities of antibodies, which they do as plasma cells. Studies in mice and non-human primates — as well as Immusoft’s initial clinical observations — suggest it is possible to administer modified plasma cells (differentiated antibody-producing B cells) without first subjecting patients to toxic lymphodepleting agents. “They engraft without any preconditioning,” says Rick Morgan, CSO at Be Bio. “We expect that to be validated in the first patient.” When transferred, modified plasma cells home to and engraft in the bone marrow, which provides them with a substantial niche. “The mechanism I don’t fully understand,” says Richard James of the University of Washington, who co-founded Be Bio with David Rawlings of the Seattle Children’s Research Institute. But, he adds, several decades of research suggest that the bone marrow niche available to antibody-secreting cells is never fully occupied. “If we put, say, 250 million more cells in, that is not going to saturate things.” Work is ongoing to establish whether other agents may improve engraftment through other mechanisms. “There might be conditioning agents that would improve plasma cell engraftment. I just don’t think it’s going to be chemotherapy,” he says. If needs be, modified plasma cells also can be redosed, although that may not even be necessary given their long survival: plasma cells persist for over a decade.
The B cell engineering concept may appear novel in terms of commercial biotechnology activity, but it has been a longstanding goal of academic scientists. Delivery of genetic cargo to B cells was a major obstacle initially. “They were refractory to lentiviruses,” says Morgan. In addition, feeder cells or human or fetal bovine serum were required to provide cytokine signals to enable B cells to expand and differentiate in vitro, but these were not compatible with good manufacturing practice requirements.
Through trial and error, different groups have come up with B cell culture systems that are compatible with their use as biofactories. These protocols support B cell expansion, differentiation and activation by exposing them at different intervals to various combinations of cytokines, including interleukin (IL)-2, IL-6, IL-10, IL-15, type I interferon, B cell activating factor and a proliferation-inducing ligand (April), as well as to CD40 and Toll-like receptor 9 stimulation.
Immusoft had long been the field’s only standard bearer. It was formed back in 2009 to license intellectual property from the lab of Nobel laureate David Baltimore at the California Institute of Technology. Baltimore, his colleague Lili Yang and co-workers developed a three-step in vitro maturation system for CD34+ hematopoietic stem and progenitor cells, which had first been transduced with lentiviral vectors encoding a broadly neutralizing antibody directed again HIV. The modified cells were then exposed to a cocktail of growth factors to skew their differentiation to a B cell lineage. The resulting plasma cells secreted the antibody at up to 1.5 micrograms per milliliter in vitro, but the protocol was never tested in patients. The original process took six weeks, which was not commercially viable, says Immusoft’s Ainsworth. The company subsequently developed a process that used isolated B cells as starting material and required just a week to produce expanded and differentiated plasma cells expressing a target protein. It has also moved away from its original lentivirus-based gene delivery platform. “We’re currently using a transposon system — we found it works very well with B cells, and it’s much easier to handle than virus,” he says. It developed its capabilities with the Sleeping Beauty transposon system through its acquisition in 2016 of Discovery Genomics. As well as providing efficient gene delivery, it also offers greater packaging capacity than adeno-associated virus (AAV) vectors. “We’ve been delivering multiple proteins from a single construct,” he says. Their method employs electroporation to deliver both an mRNA encoding the transposase enzyme and the transposon sequence containing the gene of interest. More recently, Immusoft licensed intellectual property from the University of Minnesota, which opens up possibilities in genome editing of primary B cells. Both ISP-001 and a follow-on program, IPS-002, currently in IND-enabling studies for mucopolysaccharidosis type II (also called Hunter syndrome), will, however, continue to employ the Sleeping Beauty technology.
The company expects an initial clinical readout from the trial of ISP-001 by early to mid-2025, says Ainsworth. The primary endpoint of the study is safety. Given the experimental nature of the therapy, patients continue to receive enzyme replacement therapy. Treatment interruption can only be contemplated later, when the efficacy of the therapy has been established.
Be Bio uses two distinct delivery technologies in its ex vivo gene editing process. It employs electroporation to transfer into B cells a ribonucleoprotein that comprises the CRISPR–Cas9 editing reagents. It uses an AAV vector to deliver the DNA template encoding the gene of interest, which is inserted into the B cell genome at the Cas9 nuclease cut site (the CCR5 locus) by homology-directed repair. The company reported at the American Society of Hematology last year that it can reproducibly attain a transgene insertion efficiency greater than 50%.
Be Bio is not the only company to attempt to edit B cells to produce FIX for hemophilia B. A group at Sangamo Therapeutics’ French subsidiary, which it is currently winding down, recently described an alternative B cell gene editing strategy that uses zinc finger nucleases to insert an F9 Padua sequence into the TRAC locus. The group used electroporation to transfer into the B cells an mRNA encoding two zinc finger nuclease enzymes and an AAV vector to deliver the F9 Padua sequence. In a mouse model, they detected high plasma levels of human FIX-Padua that, they state, correspond to 15% of normal human FIX activity.
Should either program progress, they would face competition from AAV-based gene therapies: CSL Behring’s Hemgenix (etranacogene dezaparvovec), which it licensed from Amsterdam-based uniQure; and Pfizer’s newly approved Beqvez (fidanacogene elaparvovec), which it licensed from Spark Therapeutics (now part of Basel, Switzerland-based Roche) a decade ago. Neither is suitable for children, however, as the therapeutic effect of the therapy, which is directed at FIX-producing liver cells, would be diluted out as they grow. Moreover, the duration of their effects in eligible adult patients is not known at this point, but only a single dose of AAV vector is feasible because of the antibody responses they elicit. “You’re effectively immunized against that class of agent,” says Morgan. The hope is that engineered B cells — which are expected to persist for many years — will bypass that problem while at the same time offer greater flexibility in terms of the dosages that can be administered to different patients, depending on their needs.
Although the list of clinical-stage programs is short, the number of proteins that developers have produced in the lab from engineered B cells is long and varied. It includes antibodies, bispecific T cell engagers, peptides, fusion proteins, and proteins implicated in conditions such as cancer, autoimmune disease, cardiovascular disease and central nervous system conditions. Given the uncertainties associated with any novel therapeutic modality, their progress toward the clinic will depend on their risk–benefit profiles.
Developing engineered B cells for conditions that are already well served is a long-term effort. James Voss at the Scripps Research Institute is working on a functional cure for HIV-1 infection by engineering B cells to produce broadly neutralizing antibodies directed against the virus. The approach goes beyond harnessing the cells’ protein-producing properties. The cells are engineered to be responsive in vivo to an immunogen or a vaccine. “A normal B cell will respond to vaccination by going through clonal expansion, germinal center maturation, and finally it will differentiate to long-lived plasma cells, which are actually going to secrete a soluble form of that B cell receptor, an antibody,” says Voss. “That’s what we want in the end is this effector antibody response.” His group does so by introducing a gene expression cassette that encodes a full light chain but just the variable region of the heavy chain, which is then spliced to endogenous heavy chain sequences. “If you use those endogenous heavy chain constant genes, that allows you to have all the normal functions of a B cell,” he says. The efficiency is quite low, but that is offset by the engineered B cells’ responses to vaccination. “One of the nice things about our approach is we do get a significant in vivo expansion depending on the immunogen that you use, and so we can get away with having lower numbers to begin with.”
His group has also contributed to an effort, led by Adi Barzel of Tel Aviv University in Israel, to develop an in vivo B cell engineering technique, which entails the simultaneous administration of two AAVs, encoding, respectively, a Cas9 enzyme and a broadly neutralizing HIV-1-directed antibody. To minimize indiscriminate DNA cutting in cells that were not co-transduced with the two vectors, the group included the guide RNA sequence with the antibody sequence, instead of with the Cas9 sequence. To further minimize off-target DNA double-strand breaks in non-target tissues, they placed the Cas9 enzyme gene sequence under the control of a B cell-specific promoter. In mice already exposed to HIV-1, the transduced B cells underwent activation and differentiation to antibody-producing plasma cells, yielding neutralizing antibody titers up to 6.8 micrograms per milliliter. In contrast with ex vivo methods, the approach is, the study authors argue, “simple, fast and cost effective,” and it does not require a match between donor and recipient. An early-stage firm, Tabby Therapeutics, is taking forward this approach, although its initial program will focus on ex vivo engineered B cells for cancer.
As yet, large pharma interest in this emerging area has been minimal. Takeda, of Osaka, Japan, entered an alliance with Immusoft back in 2021 that was focused on engineering B cells for central nervous system applications. However, it exited the relationship about one year ago, when it terminated all early-stage gene therapy research, says Ainsworth. “We do continue to work on that,” he says. There is appetite for deals, but the initial programs need to mature first. “I think clinical data is going to be the big driver. Showing that we can deliver this safely and efficaciously — that’s going to be key,” he says.
In the meantime, the failure of Walking Fish Therapeutics to raise new financing to advance several preclinical programs may cast a pall over this nascent but promising niche. The company, which closed a $73 million series A round in February 2022, had reached late preclinical development with a lead program in Fabry disease before shutting down. Investor apprehension is commonplace in biotech innovation. The field of engineered B cells is not yet, in venture capital parlance, de-risked. But for those willing to back the technology, the rewards could be substantial.